The fatal gaps after rehab haunt the doctor who tried to save him.
His mother’s words are piercing and permanent, burned into my broken heart. I stare at her in awe, my tear-filled eyes unblinking. She stands in daring pink; we listen in solemn black. My legs want to buckle. How does she find the words? How do they travel from her tired brain, past the lumps in her throat, and out her quivering mouth? Out through lips that will never touch her son’s cheek again.
And the words that follow also cannot begin to adequately convey my thoughts and feelings about my boy. This is not a task for any mortal. And certainly not one for a mother. But here goes: Philip …
Philip was my patient. I believed I could help him change the trajectory of his life. I believed in him.
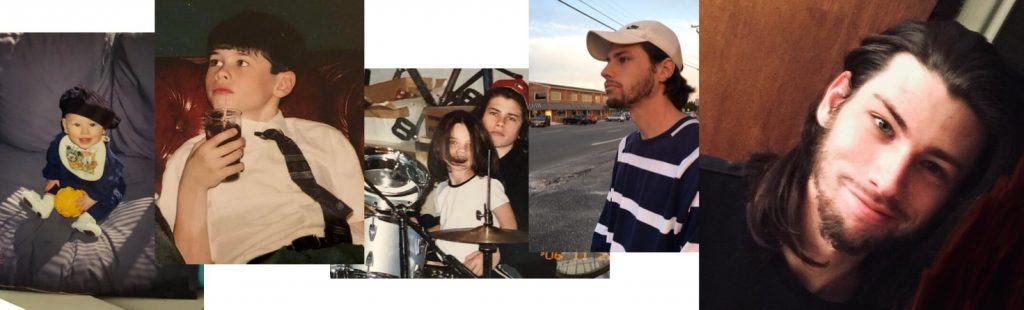
In 2016, the amazing shock of coffee brown hair first appears in my office. It makes such an impression, I stare at it for a few moments longer than might be considered polite. The mane belongs to a 22-year old man-child so easy to talk to, so honest about his history in and out of outpatient treatment for addiction, and far too comfortable with his opiate use: heroin and a couple of benzos. Every day.
“Yo, doc,” Phil says, with a little smile, a lot of charm, after flopping casually onto the couch. “How’s it going?”
“You tell me,” I answer.
I’m Dr. Aviva, a physician who is board-certified in Addiction Medicine and Family Medicine. Patients don’t call me by my last name. In Hebrew, Aviva means spring. Just like the season, spring forces us to see life in a new way. I want the same for my patients. New life also brings hope. I have every hope for Phil.
Now that Phil is seated, my bespectacled eyes meet his. I give him a wry smile, but I don’t waste time with small-talk. A single mother with three children of my own, I run a tight ship. One of my patients once told me that my super power is seeing directly through bullshit.
“Keep it moving,“ Phil says. It’s his motto, his mantra, his crutch. “Just keep it moving.”
Until he doesn’t.
Philip … loved so deeply. He took great pride in his brother and sister and their accomplishments. And damn it, he didn’t intend to cause you two this pain. But that other side of him defied his better self.
He loves them. I know this by the way he talks about them using nicknames. But he is ashamed by their progress and his stagnation. Drug use has put him at least one decade behind his siblings.
“… when he overdoses in the middle of the suburban Philadelphia shoe store he manages, his collapse captured on surveillance camera, he finally decides that his condition is serious.”
This is the true story of a failed recovery, told through a mission to save a life, and an enduring optimism that change can happen. It is why his mother’s eulogy haunts me. A mother who white knuckled her way through the last ten years and felt in her gut that addiction would take him. I was determined that it would not.
Not that Phil failed. Not at all. Phil tried with every fiber of his being to survive. He wanted therapy to work. He wanted a better job. He cherished his grandparents. But he struggled with demons: anxiety, depression, and genes. In the end, when it mattered most, Phil slipped through the gaps in the medical system: the one that can and does produce miracles. Every day it revives a young man who overdoses, provides him a warm hand-off to treatment, follows him closely when in-patient care has ended, responds to relapse, and keeps him connected to a team of doctors, therapists, support groups, and healthy relationships with family and friends. That’s when the medical system is seamless. But when it’s not? When there are gaps? Treatment and supports can’t be over at the exit door. Three to five years of support need to be mapped out, with a stepped down approach. What’s unclear: who is responsible for setting up that care model? The residential provider who treats and releases? The primary care physician? The family? Gaps mean patients can fall hard. Like Phil.
I know I have tried to make sense of this wonderfully smart and spirited and beautiful and talented, passionate, and loving boy, who also had aspects of darkness, of fear, of vulnerability, of some complicated force within that pulled him towards roads he couldn’t navigate himself away from. Always. Philip was complicated and let’s face it, he could be a little difficult. Damn, his birth was complicated and difficult.
Just like addiction. Complicated and difficult.
Phil dabbles in outpatient treatment. He doesn’t go through rehab, or detox and he’s tried Suboxone, an FDA-approved oral medication for opioid use disorder, but not under my watch. He has friends, relationships with both of his divorced parents and two siblings. Plus, a job at a shoe store, where he is more than a manager. He is a legal hustler, a clever money-maker, continuously coming up with creative ways to bring in extra cash. He selects the highest-end shoes and sells them without hesitation. He tells me all about it with a twinkle in his blue eyes.
But in 2018 when he overdoses in the middle of the suburban Philadelphia shoe store he manages, his collapse captured on surveillance camera, he finally decides that his condition may be serious. And the shame he feels pierces deeply.There is no “one-size-fits-all” approach to treatment. The only universal truth may be that very few people who struggle with a substance use disorder will ever be “cured” in 30 days. There is no possible cure for a chronic disease in a mere 30 days, no matter what it is. If it were that easy, we wouldn’t be losing close to 200 loved ones every single day to drug overdose. Add alcohol to that mix, and we lose 400 Americans every day. Many of them are transported to our emergency rooms. The American medical system has countless hours of experience dealing with the addiction crisis.
One of his best friends overdoses on heroin, survives, but because he is immobilized and alone for too many hours, he loses a leg.
And yet … consider this. An ER nurse knows, by heart, the step-by-step protocol for a patient who comes in with the Ebola virus, an extremely rare occurrence in the U.S. And take a common occurrence, like a heart attack. Go into 99 emergency departments in 99 hospitals, and you’ll find almost 99% consistency in both your cardiac workup and aftercare. Why don’t we have that for substance use disorder (SUD)? Where are the rock solid steps for the patient who overdoses, who relapses, who “finishes” treatment? And even before a life-threatening emergency, where are the standardized treatment protocols to recognize and treat the person who is misusing their prescription medications but is working, maintaining a job and relationships, and can still afford a vacation? So often, people who struggle with an SUD look fine on the outside. Their symptoms are hidden. But unaddressed, they can and often do escalate, and lead to emergencies.
As cool as he appears, Phil is scared. One of his best friends overdoses on heroin, survives, but because he is immobilized and alone for too many hours, he loses a leg. He is 21 years old. He’s one of my patients too.
Philip had great charm, charisma and an ironic sense of humor. These qualities made for a period of his great success in sales. He read people well and could talk them into buying things they didn’t even know they wanted. He quickly rose from sales associate to store manager. How proud he was! And that hair! That infamous beautiful head of hair that was like a trademark, that accented his blazing blue eyes and incredibly handsome face. He knew it, yet at the same time he was quite humble and shied away from center stage.
Doctors aren’t supposed to have favorite patients. They’re supposed to treat everyone with the same level of care, do no harm, no matter how difficult, irritating, or manipulative a patient might be. Addiction Medicine doctors get more of their fair share, because more often than not they are dealing directly with the hijacker inside the patient’s brain. That powerful, relentless, suicidal hijacker who convinces the brain that the drug is more important than food, water, shelter, and relationships. A hijacker that takes aim and re-hardwires the reward and pleasure center of the brain while simultaneously de-activates the thinking, reasoning, consequence-understanding frontal lobe.
But Phil is one of my favorites. His charm, his grin, his unforgettable hair – he gives me hope. I prescribe him oral buprenorphine, but am worried about his compliance. We talk about trying Sublocade, an injectable, long-acting form of the medicine designed to treat substance use disorder. The complexities of prior authorizations and out of pocket costs make that insurmountable as an option. With an injectable, I know he has the medicine on board for a month. Oral medications rely on consistency and compliance with daily dosing. Pharmacies can autonomously switch out any generic prescription, but different brands of the same medication have different percentages of active ingredients, so the same drug can vary widely. With SUD, a different generic brand may have different potencies. Lower strength medicine can make a patient suffer from withdrawal symptoms. It can present as the patient needing more medication, and taking more medication. It doesn’t allow for consistency and reliability, which a patient with SUD so desperately needs. Even the drug dealer on the street corner doesn’t like to dole out unpredictability.
Phil gives off a vibe that things are getting better. But then his urine screen comes back positive for drugs. We discuss yoga, meditation, group meetings, getting away from the old crew, most of whom are using, some of whom are my patients. But the overall feeling he gives is this: I want to do better. Keep it moving, doc.
He was known for his musical talent. What a gifted and amazing drummer, winning out older kids in middle school to be selected for the competition jazz band. I cherish the days when he’d come home from school and head immediately downstairs to play his heart out, as if he’d been waiting all day to do so. I recall his very accomplished drum instructor telling me, “He’s scary good” and recommended him to a music school in NYC because he was exceeding his capacity to teach him. But that same damn other side was an obstacle not to be overcome, and he did not pursue.
Phil steals his dad’s beloved instruments, pawns them, and confesses to me. He looks down at the floor as he tells me. He knows exactly how important those drums are to his dad. And then he admits what I already know: he’s using heroin again.
It’s March 24, 2019, and Phil and I have a breakthrough. It’s not pretty.
“You’ve never been inpatient, Phil.” I meet him where he is. “You have to try.”
“I don’t need inpatient. I’m good.”
“Okay. Give me a urine sample, just to be sure,” I say.
Phil refuses.
“I’m here of my own free will.”
His entire affect changes. He’s wildly angry. He stands up and hovers aggressively, looking down nearly a full foot to meet the eyes behind my bold-framed glasses. His brain is hijacked. He is anything but free.
“Come on, Phil. This is b.s. Let’s do this.”
Phil storms out of the room and slams the door. This time, something happens to my brain; a struggle between Dr. Aviva the physician and Aviva the mother. Phil’s on the tracks. And I instinctively want to fling my body in front of that oncoming freight train. I do something I’ve never done before – open the window in the exam room, and yell across the parking lot. Like he’s my kid.
“Hey! Come back in here, this is bullshit! Let’s finish this!” It’s a risk.
“What kind of fuckin’ doctor are you?” Phil screams back. “You can’t talk to me that way!”
He storms off across the parking lot. It’s not paying off. He can’t hear me. It’s like he’s drunk. Here’s this amazing, brilliant kid, and his brain just can’t compute. I find Phil’s mom still standing in the waiting room and admit to her all I’ve said. She gets the urgency. And she thinks he will leave with his dad. I dart out to the parking lot and see Phil’s dad’s car. I walk quickly to the driver’s side window.
“What’s going on here?” I ask Phil. He’s sitting in the passenger seat, staring stonily out the window.
“I’m done. There’s nothing to talk about.”
I turn to dad. “What do you think?”
“I think enough is enough and we have to do something,” dad says.
“Listen, with all due respect, you have to give him an ultimatum,” I am still talking to dad, knowing Phil can hear every word. “He needs in-patient care. I’m not a tough love person. I’m not. But you can make this happen. You’re not kicking him out. You are presenting the choices to him. He can decide what he wants to do. “
It’s like convincing a toddler. Not, do you want to brush your teeth? Rather: you can get dressed first or brush your teeth first. You choose. Except the adult version here might mean the difference between surviving and not. Between life or death. Phil is glowering, about to explode. I am almost embarrassed that I’m so emotionally involved. But if it were my son … Phil opens his mouth, and the hijacker speaks.
“You just want the money. You don’t give a shit about me.”
That front part of his brain, the rational, consequence-understanding, thinking part? Not activated. He’s teetering between fight and flight. That’s it.
“Really Phil? That’s what you think?” Now I’m pissed. “I don’t get paid to stand out here in this parking lot on a beautiful Sunday afternoon. I’ve got three kids at home. But I’m here because I know you need this. I know you want this. Remember what happened in your shoe store? You want that to happen again? You’re really okay with that? This is how you keep it moving?”
Phil looks me in the eye. He hears me but says nothing.
“I don’t give a shit about the money,” I say. “In fact, I can’t keep taking your parents’ money if you don’t do this. It’s not ethical.”
“Just go,” Phil instructs his dad. They drive off.
Less than an hour later, Phil’s dad sends me a text. Phil makes his choice. He packs up slowly and leaves the house.
“I am so scared,” his dad texts me. I am too.
“I will check in with you. On a regular basis,” I write back.
At three years old, Philip was chasing his friend Elias on the playground, who had adeptly scrambled to the top of a jungle gym. Wanting to retaliate for some three-year-old act of injustice, he ran to me with arms open, “Mommy, will you carry me to the top of the jungle gym so I can hit Elias?” I was so struck by those opposing forces, his primal determination accompanied by his fear of the physical challenge. That interchange is emblazoned in my brain as if it was yesterday. Two sides of Philip that just never quite seemed to resolve. His determination to meet a goal, and his fear of the challenge that was required to get there.
Determination. Fear. Determination. Fear. Monday morning at 4 a.m., Phil comes home. He’s cold. He will go to rehab. He immediately gets into a recovery program at an in-patient facility right down the road. Great. But insurance won’t cover it. Shit. He enrolls in the same organization’s recovery program, but in another state, insurance dictating where he can or can’t go … and then …
Phil disappears into the gap. I try to reach him. I call the center to get in touch with his counselor. I’m given another phone number which ends up being the woman in charge of placement, who wants to send me to someone else. It’s a maddening maze.
“I sent my patient to you,” I argue. “I’m trying to coordinate his care.”
“I’m just in charge of prior authorizations. I’m not the right person.”
“Get me the right person.”
Phil is in a crevasse, and I can’t throw down a rope. I am the referring doctor. I got him in there. In past experience, there is always communication between the doctor who refers the patient and the primary therapist. Not this time. Phil refuses to sign a release to communicate with his parents, with his doctor, with anyone. Too many silos. I keep calling. Keep it moving.
Finally, after a week of trying, I reach a therapist at the facility who says Phil’s doing okay. But he’s not on medication-assisted treatment, the FDA-approved drugs for opioid use disorder. What about detox? What about the injectable medication vivitrol? There’s no information. There’s no communication. The therapist shares nothing. But, hey, he’s in there. He’s not out in the cold. He’s getting help.
At the end of the month, I take a rare leave from the office to go to the Heroin and Prescription Drug Summit in Atlanta. It’s a gathering of the great minds in addiction medicine. The head of the National Institutes of Health is there. The chief scientist of NIDA (National Institute on Drug Abuse) is there. For the first time in the summit’s history, a sitting President and First Lady appear together, putting a double exclamation point on the suffering affecting American families every day.
I have one word for the chart notes kept on Phil while in treatment: pitiful.
I meet a group of women at the summit, and like four magnets, we connect. It’s immediate and powerful. One is a judge responsible for revamping an inner city drug court. Another is running an anti-stigma campaign in Canada. Another is a former news anchor who left journalism to take on the addiction crisis. They are sharing war stories, and I share the story of this special patient who’s on my mind. I confess how I yelled out the window and chased him down in the parking lot. I still can’t believe how I Iost my cool. But I couldn’t let him walk away. In ten years of private practice in Addiction Medicine, I’ve lost three patients. Each one takes a piece of me that I’ll never find again.
“I believe in this kid,” I say with an enormous smile. “He gives me hope.”
What I don’t know: Phil is already gone.
To his good friends of many years, please know that I understand how difficult this is for you. This is not a loss that should be woven so early into your history.
On April 24th, it’s the last day of the conference. Phil’s mom calls to let me know. Heroin. An overdose. Shock. He was discharged from rehab with no follow up scheduled. Anger. He had been told to go to IOP – intensive outpatient program, but insurance would not cover it. Disbelief. The memorial service is this weekend. After she hangs up, I let the tears fall. He was so damn close. He wanted to keep it moving; he really did. Sadness. Profound sadness.
And then I say out loud to the universe, “I am going to find out what the f*&% happened.”
But first, I have a eulogy to hear.
I can feel deep inside of me that I will someday make greater sense of this, of losing our beautiful boy too too early. And I hope the same for every dear friend and family member in this room, all of whom are so deeply saddened along with us. I so hate the pain our family is inflicting on you. Yet, the words written to me by my dear friend soothe me. “It creates an interconnectedness and a loving energy that is transmitted to a widening circle with Philip at the center, as his life and your family have touched so many”. I love that.
We are mother-to-mother again, just like in the waiting room, and I am deeply moved by her words. I sincerely doubt I would have the same strength, grace, and poetry under such duress. I, too, want to make greater sense of this, not just for one mother’s son, for this family, but for all the Phil’s — and the families that love them — who fall in the gaps.
I call the clinical liaison from the treatment center that helped get him in there. I get the permission I need to call the rehab facility and retrace the missteps. I already know that their lack of communication with me while he was there was a problem. But I want to know what happened after they released him. Usually a patient has insurance coverage for at least 30 days inside this treatment facility, but Phil is discharged after just 21 days, on April 15. He goes home to his dad’s house. He attends a few “Rehab After Work” meetings. He calls them “a joke” and the group facilitator “a clown.” Nine days later, he overdoses on heroin for the last time.
The records show that Phil had declined to give me access to him. The records don’t show that Phil’s mom tells the treatment center to contact me, many times. The counselor notes that Phil hasn’t seen me for two months. It’s untrue, I am the one that referred him there but the counselor takes him at his word. There is no fact checking or calling me, the referring physician, to get more information. She encourages him to seek intensive outpatient treatment, but insurance refuses to cover it. If not, Rehab After Work three days a week, and AA meetings every day. Make an appointment with his doctor. No mention of any medication-assisted treatment for opioid use disorder. No details about what interventions he gets in rehab. No suggestion for the full-wrap around services, with a therapeutic community in a recovery house. No appointment for family therapy. No description of the “family therapy” session which is more of a discharge planning meeting, not led by the therapist who worked with Phil for three weeks, but by a therapist who has never met him. No discussion of a trauma that impacted Phil while he was in treatment: a counselor involved in Phil’s care relapses and dies.
I have one word for the chart notes kept on Phil while in treatment: pitiful.
The clinical liaison from the treatment center calls me back. I resist a genuine urge to scream and curse at him. He is not aware of Phillip’s death. He is not aware there was no follow up appointment. He is not aware that Phil was sent out with no life-sustaining medication. I blame him for the wide gap Phil fell into. But I say it differently. He understands. He apologizes. He connects me to the clinical director who hears me out, and promises to make changes. We are going to work together. We are going to develop protocols for care after a patient is released.
They don’t have protocols? Do they know there’s an opioid crisis in this country? That’s a giant gap. We must fill in the gaps.
I call an administrator at the facility. I refer a lot of patients to them. They can do good work. Not this time. “I sent him to you. And you sent him back into the world. Why wouldn’t you tell me?”
Consider a knee replacement. Appointments with the physical therapist aren’t optional; they are assumed and set up immediately. Follow-up appointments with the orthopedic surgeon are scheduled. People drive you around, bring you meals and meds. Why can’t we do this with the disease of addiction?
Patients on opiate-blocking medications like Buprenorphine/Suboxone don’t overdose. They can’t overdose. They don’t die. They do not die.
Phil calls it pitiful too. When his mother visits him in rehab, he wears a green long-sleeved t-shirt that make his bright blue eyes sparkle on his sun-kissed face. He’s looking strikingly handsome. The healthy Philip, his mom thinks and wants so much to believe.
“See that guy?” Phil tells his mom as he points across the room. “This is his 9th rehab. And this guy? His 22nd.”
Looks are deceiving. His cheeks are flush, his blood pulsing powerfully, his brain engaged, his body fully alive. But he is drowning in hopelessness.
“Phil, I’m so afraid you are going to die,” his mother says.
“I won’t. I promise.”
The shock is slow to wear off. When Phil’s mom tells me about his death, my headspace assumes Phil is still in-patient, getting treatment, making progress. Rehab can be such a good reboot. I see it work, over and over. Addiction is a chronic disease, like diabetes – you don’t get over it, you manage it. It doesn’t define you – but it’s forever part of you. Phil’s never gone on this trajectory before. This is a part of the treatment continuum he hadn’t explored. And when he does get out, he will follow up with me. I don’t consider the possibility that he won’t. I never dare to consider that he’s released too soon. Without a word. No phone call, no follow-up appointment, no communication from the center. The hours and days immediately after treatment are the most vulnerable times for patients struggling with addiction. But whenever he does get out, I also know he’ll be on medication, right? Patients on opiate-blocking medications like Buprenorphine/ Suboxone don’t overdose. They can’t overdose. They don’t die. They do not die.
I know the last thing Philip would want would be to leave us being sad. I know this. I KNOW this is not what he wanted. But it was also something, dammit, he just couldn’t fix. This walking dichotomy that he was, just couldn’t find his place in peace. I sure as hell hope he has now. Philip so deserves that place in peace, and we deserve some tiny ounce of comfort in knowing that perhaps, just maybe, our beautiful boy has found that.
I lost him. But somehow, I have to keep on moving.
___________________________________________________________
The authors, Dr. Aviva Fohrer and Kimberly Lohman Clapp, met in 2019 at the Rx Drug Abuse & Heroin Summit. Dr. Aviva practices Addiction Medicine outside of Philadelphia, PA. Clapp (on air: Suiters) was an Emmy-award winning journalist and the former Senior Director of Communications for SAFE Project.
